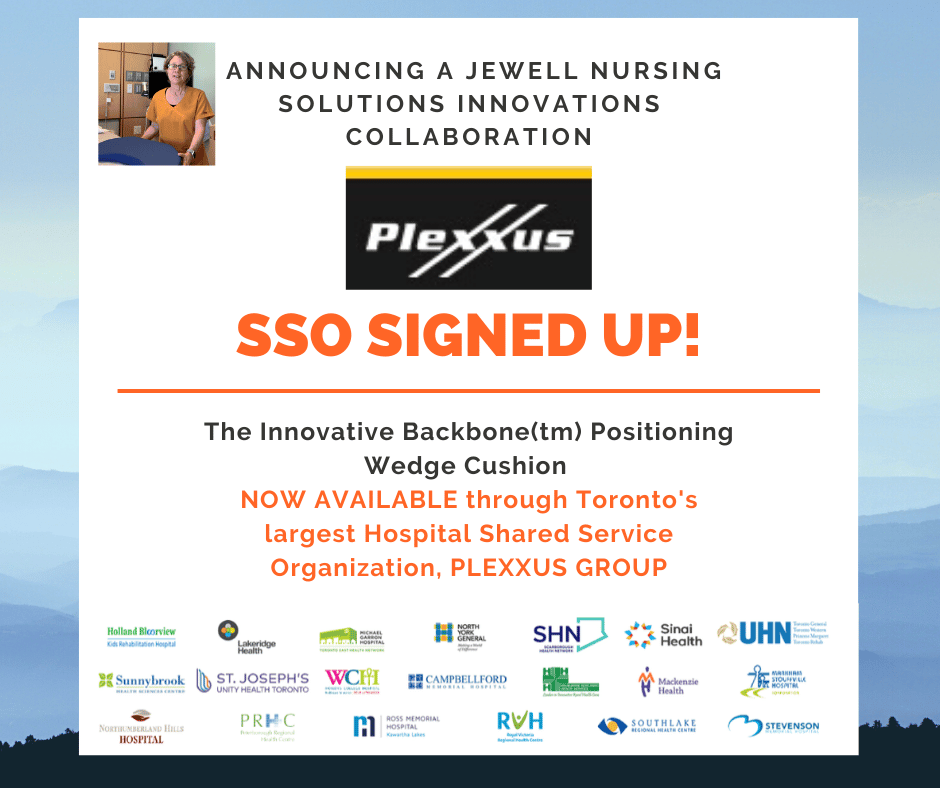
Why I got into the pressure injury prevention biz
My Scope of Practice: Take a Load Off
By Barbara Zeiger, originally published in OWM Journal May 5th, 2017
Gwen Jewell, RN, BSN, CWS, often asks herself why she is so obsessed with creating the perfect offloading devices. Inspired to undertake a medical career after her younger brother suffered a spinal cord injury that left him quadriplegic, Gwen pursued an interest in research that morphed into a passion for patient care that morphed the desire to improve support and positioning products.
After her brother’s accident, Gwen found a job as a secretary at a small biotechnology research company (DNAX, Palo Alto, CA). “It was perfect,” she says. “I could immerse myself in a research environment while I took prerequisite courses at local community colleges in my area — whichever college offered the course, at night, on Saturdays, or online, wherever I could get the course I needed. In all, I attended 7 different community colleges over 4 years. I felt it was important to develop skills in both patient care and science, so also I obtained certifications in phlebotomy, biotechnology, and medical assisting.”
The phlebotomy skills she developed put her on a fast track into both patient care and research. She landed a part-time job at Genentech, Inc (South San Francisco, CA) in their onsite Occupational Health Clinic. “I was hired to perform phlebotomy services for their research blood program and assist with their employee medical surveillance and robust employee ergonomic safety programs. It was a perfect fit for me because I could simultaneously learn hands-on medical care and research and still have time to finish my prerequisites.”
At Genentech, Gwen worked with a team of dedicated occupational nurses, including Diane Fuller, RN, BSN, COHN, and Anne Tsolinas, RN, BSN, COHN-S. “They were wonderful,” Gwen says. “They provided guidance and encouragement and helped me see my passion, strength, and potential came from direct patient care more so than research. I realized that if I was a nurse, I could make a difference every day, not just someday. I shifted my education toward qualifying to get into nursing school and was accepted to San Francisco State University School of Nursing, graduating in 2006. Upon graduation, I started working at the Dignity Health Sequoia Hospital Medical Surgical Unit [Redwood City, CA], and I have never looked back.”
Gwen’s interest in wound care and patient bedside ergonomics began fairly early in her nursing career. Shocked by the Stage 4 pressure injuries of a patient transferred from the emergency room, Gwen wondered why the wounds could not have been prevented. She says, “That incident inspired me to study wound care because I wanted to learn how to treat wounds like this and especially because I realized learning how to prevent them is more important. I began my journey of pressure injury prevention the next day by joining our Hospital Acquired Pressure Ulcer (HAPU) Prevention Committee, under the experienced leadership and guidance of Lynne Grant, MS, RN, CWOCN.”
Gwen recognized the greatest need for improvement and potential for contribution was to advance the science of pressure offloading. She started designing offloading devices because she felt the products available were uncomfortable or ineffective and the science to support the offloading/positioning technology was lacking, with little consideration for the relationship between the ergonomics of the severely immobile patient and pressure offloading needs when in bed.
“My first project in pressure ulcer prevention device development was a heel floating device I called ‘The Heelbone,’” Gwen says. “I targeted heel floatation first because it was easy to see why other devices did not work. I determined devices should provide 100% pressure reduction for all the bony prominences of both feet, including the heels, malleolus, and metatarsals, regardless of what position the person’s legs might be in and without restricting movement or forcing the person into an uncomfortable or unnatural position. The device would not catch, tangle, cover, or be cumbersome to apply. The device could be used by any patient, for as long as they need it, in any care environment, and would be comfortable for everyone. Laughably, I thought creating this ‘perfect’ device would be easy.”
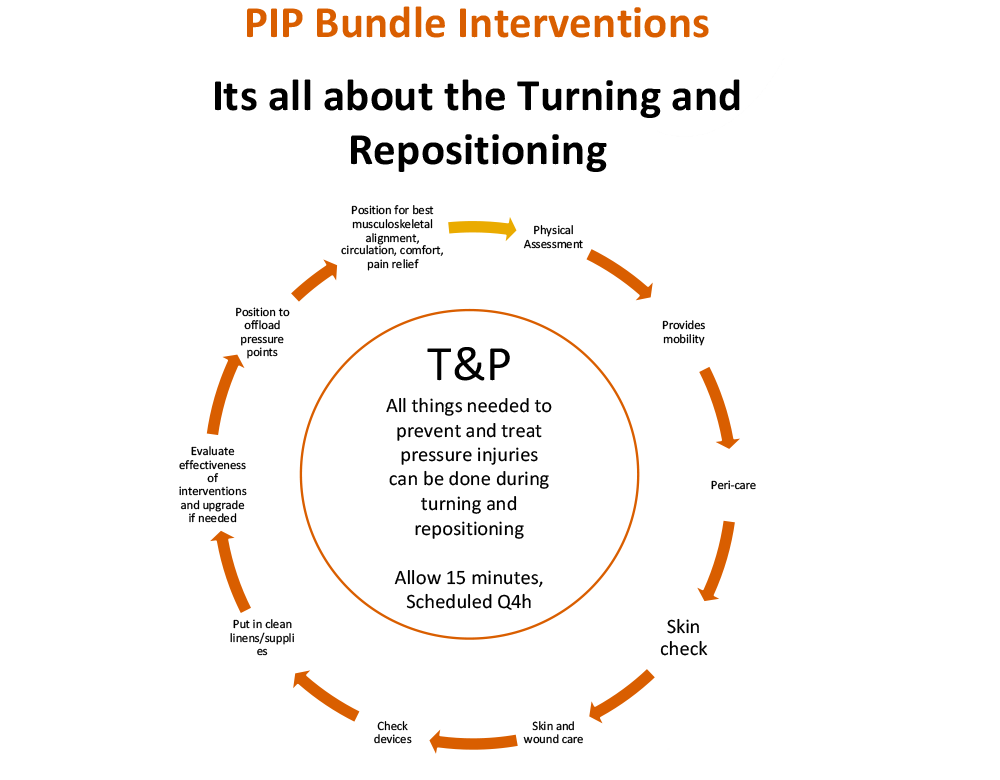
In 2014, Gwen was appointed a MeasureVentionist for the national No Harm Campaign. She and colleague Micaela Gonzalez, RN, BSN, composed and implemented a bedside teaching program for pressure injury prevention in their hospital. These responsibilities helped Gwen connect the dots between the physical and behavioral needs of a bedbound person and effective pressure offloading. “I began to teach our caregivers to watch for spinal alignment and position to promote maximum circulation,” Gwen says. “Rather than focus on boosting techniques, we looked for techniques to minimize slide during head-of-bed elevation and how to turn and offload the patient in a semi-Fowler position without compromising thoracic capacity or creating awkward twisting. And, of course, we taught how to offload the bony prominences effectively.”
All of these concepts involved using something to support the patient, but the devices available fell short for one reason or another. “When it came to 30˚ lateral turning, I determined that in order for a device to be ‘perfect,’ it would have to provide 100% offloading of the sacral area while helping to maintain an ergonomically correct position,” Gwen says. “It also would have to be very stable or the patient would not stay offloaded for long. Most importantly, I was back to my defining nursing principal — ie, that comfort is key to effective intervention. Again, I was sure that designing such device would be a piece of cake and that by next week or so I would have something that would cut pressure injury incidence by half at least! It only took me 3 years and 6 prototypes later to come up with The Bedsore Rescue support wedge [Jewell Nursing Solutions, Redwood City, CA].”
Gwen feels victory and satisfaction in seeing that patients are in better shape at the end of the shift than how they were when she started. Although she admits it is somewhat self-serving, she enjoys taking credit when patients breathe a sigh of relief or say they feel better because of whatever she did or said. “On another note, my efforts are self-serving because I get irritated when I have to use or do something that just doesn't work well,” she says. “But in the bigger picture, as cliché as it sounds, it is important to me to believe my nursing career has contributed to the greater good. When the day comes I can no longer be a nurse, I want to be able to say that I left health care in better shape than it was when I started. I now find myself on a quest to get my creations into the hands of people who really need them, both because I want to help reduce suffering, and also to be successful in my life’s contribution.”
Gwen says she has always been in awe about the wonders of medical science, both from a physiological perspective and for advancements we have achieved. “I think one of the most significant truths about health care today is that most of the time, we don’t cure people, we mend them.” With her innovations and dedication, Gwen aims to foster an environment where the body can best heal itself in her scope of practice.
This article was originally published in the OWM (Ostomy Wound Management) journal on May 5th 2017 written by Barbara Zeiger. See more from OWM here: